An ectopic pregnancy or tubal pregnancy is when the fertilized egg implants outside the uterus. Most are in a fallopian tube, but occasionally the egg may attach elsewhere, such as in an ovary, in the cervix or other places in the abdomen.
The narrow fallopian tubes are not designed to hold a growing baby, so the fertilized egg in a tubal pregnancy cannot develop normally. Eventually, the thin walls of the tube stretch to the point of bursting. If that happens, it is potentially life-threatening for the woman, because of the high risk of internal bleeding and hemorrhage. If the tube bursts, it could destroy it’s ability to carry fertilized eggs on their way to the uterus in future pregnancies.
What Causes An Ectopic Pregnancy & Who’s At Risk?
Most ectopic pregnancies are caused by the inability of the fertilized egg to make it’s way through a fallopian tube into the uterus. This is often caused by infections such as a ruptured appendix or an inflammation caused pelvic inflammatory disease (PID), which can cause the tube to become party or entirely blocked.
Scar tissue left behind from a previous infection or abdominal surgery may also interfere with the egg’s movement. Also, a condition called endometriosis; where bits of tissue (the tissue that lines the uterus) escape the uterus and become implanted on other pelvic organs- can cause scar tissue to block the fallopian tubes. This can interfere with conception or prevent the fertilized egg from arriving in the uterus.
Another possible cause of ectopic pregnancy is an abnormally shaped tube, which may be the result of abnormal growths or even a birth defect.
The majority of ectopic pregnancies occur in women over 35 and women who have had previous ectopic pregnancies. Also, the use of an intrauterine device (IUD), surgery on a fallopian tube, several induced abortions, infertility problems or medication taken to stimulate ovulation increases the chances of an ectopic pregnancy.
more on Ectopic Pregnancy
—Symptoms of Ectopic Pregnancy?
—Ectopic Pregnancy Diagnosis
—After an Ectopic Pregnancy
—Treatment of Ectopic Pregnancy







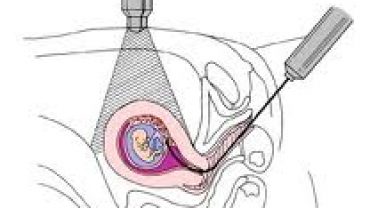
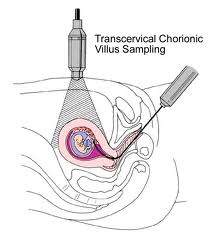 Chorionic villus sampling is usually done early in pregnancy between the 9th and 13th week. This is a procedure that involves removing a sample of chorionic villi cells from the placenta at the point where it attaches to the uterine wall.
Chorionic villus sampling is usually done early in pregnancy between the 9th and 13th week. This is a procedure that involves removing a sample of chorionic villi cells from the placenta at the point where it attaches to the uterine wall.
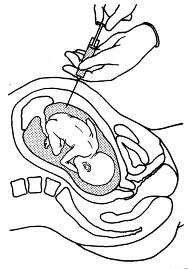 The amniocentesis test is a test in which a needle is used to remove a sample of fluid from the amniotic sac surrounding your baby. The amniotic fluid, which contains cell shed by your baby, is then studied in a lab for analysis. If done for chromosome analysis, amniocentesis is usually performed after the 16th week of pregnancy. If a woman needs to give birth early for some medical reason, amniocentesis might be done shortly before delivery to asses fetal lung maturity.
The amniocentesis test is a test in which a needle is used to remove a sample of fluid from the amniotic sac surrounding your baby. The amniotic fluid, which contains cell shed by your baby, is then studied in a lab for analysis. If done for chromosome analysis, amniocentesis is usually performed after the 16th week of pregnancy. If a woman needs to give birth early for some medical reason, amniocentesis might be done shortly before delivery to asses fetal lung maturity.
