Most couples are advised to wait until they have been trying to conceive for at least a year, before seeking medical help, with the exception of couples over 35. Those that are over 35 or those that have reason to believe there may be a fertility problem should not wait a year before consulting a doctor.
Infertility testing and treatment can be difficult and expensive. Before starting infertility testing, it’s best for couples to discuss how far they would be willing to go with testing and treatment. Only have testing for conditions that they are willing and financially able to have treated would help them move on to other options such as adoption.
Diagnosis of infertility may take the use of a special doctor called an infertility specialist or a reproductive endocrinologist. Infertility is diagnosed after an infertility workup, which includes a physical exam of both partners to determine their general state of health. Many times, laboratory tests are conducted and sometimes both partners are interviewed about their sexual habits in order to determine whether intercourse is taking place properly for conception. If no obvious cause can be determined at that point, like improperly timed intercourse or absence of ovulation, more specific tests may be recommended.
Depending on the test results of those tests, different treatments can be suggested. About 90% of infertility cases are treated with medication or surgery. Various fertility drugs may be used for women with ovulation problems. It’s important for couples to talk with their doctor about the drug to be used, so they understand the drug’s benefits and side effects. An x-ray of the fallopian tubes and uterus may be done after dye is injected, to show if the tubes are open and to show the shape of the uterus. An exam of the tubes and other female organs for disease may be done, using an instrument called a laparoscope to see inside the abdomen. If needed, surgery can be done to repair damage to a woman’s ovaries, fallopian tubes, or uterus.
For a man, testing usually begins with a semen analysis, which looks at the number, shape, and movement of his sperm. Because semen is rather variable in quality, the test may be repeated. Sometimes other kinds of tests, such as hormone tests, are done.
Depending upon the degree of abnormality, the treatment may range from relatively simple artificial insemination of the woman with the man’s semen (AIH), through conventional in-vitro fertilization and embryo transfer (IVF-ET), to the latest techniques of assisted fertilization by microinjection (ICSI). In infertile couples where women have blocked or absent fallopian tubes, or where men have low sperm count, in vitro fertilization (IVF) is an option. In IVF, eggs are removed from the ovary and mixed with sperm outside the body in a culture dish. After about 2 days, the eggs are examined to see if they have become fertilized by the sperm and are dividing into cells. These fertilized eggs (embryos) are then placed in the women’s uterus.



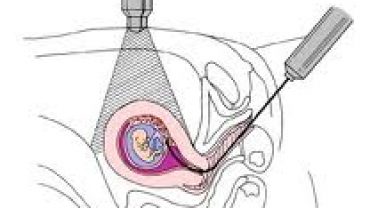
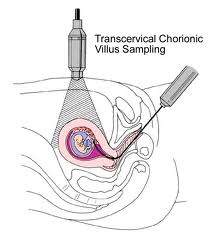 Chorionic villus sampling is usually done early in pregnancy between the 9th and 13th week. This is a procedure that involves removing a sample of chorionic villi cells from the placenta at the point where it attaches to the uterine wall.
Chorionic villus sampling is usually done early in pregnancy between the 9th and 13th week. This is a procedure that involves removing a sample of chorionic villi cells from the placenta at the point where it attaches to the uterine wall.
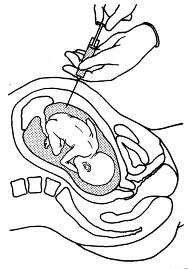 The amniocentesis test is a test in which a needle is used to remove a sample of fluid from the amniotic sac surrounding your baby. The amniotic fluid, which contains cell shed by your baby, is then studied in a lab for analysis. If done for chromosome analysis, amniocentesis is usually performed after the 16th week of pregnancy. If a woman needs to give birth early for some medical reason, amniocentesis might be done shortly before delivery to asses fetal lung maturity.
The amniocentesis test is a test in which a needle is used to remove a sample of fluid from the amniotic sac surrounding your baby. The amniotic fluid, which contains cell shed by your baby, is then studied in a lab for analysis. If done for chromosome analysis, amniocentesis is usually performed after the 16th week of pregnancy. If a woman needs to give birth early for some medical reason, amniocentesis might be done shortly before delivery to asses fetal lung maturity.
