Diet is the best tool to minimize morning sickness discomfort and make it more bearable. Sometimes you may reduce nausea and vomiting by making changes in your diet and eating habits.
Keep a few simple snacks by your bed, such as soda crackers, graham crackers, granola bars, rice cakes, dry cereal or pretzels. Eating carbohydrate-rich foods and foods high in protein, especially right before you get up in the morning, may help combat nausea. Nibble a few crackers and then rest for 20- 30 minutes before getting out of bed. Snacking on crackers may also help you feel better if you wake up feeling nauseated in the middle of the night.
Due to increased estrogen levels, pregnant women are particularly sensitive to smells. Try to avoid the sight, smell, and taste of foods that bother you and make you queasy. Many pregnant women want to avoid any activity that has to do with food when they are feeling sick, including cooking meals and grocery shopping. Have your partner prepare meals and shop for food, when possible. Also, when cooking (or when your partner is cooking), make sure to keep windows open and have a fan on to minimize food odors that might trigger nausea.
The nausea experienced during pregnancy is one of the few that is relieved by having food in the stomach. Eat before nausea strikes, because food will be easier to get down and that way, you may be able to prevent an attack. Eat small, frequent meals or snacks throughout the day (as often as every 1-2 hours if necessary), so that your stomach is never empty, since an empty stomach tends to make morning sickness worse. Low blood sugar levels, resulting from long stretches between meals, can trigger nausea, as can eating too much at one meal. Large meals are to be avoided.
Women with a higher intake of fat may be more likely to suffer morning sickness than those with less saturated fat. Limit or eliminate fatty, greasy and fried foods, which take longer to digest, particularly during pregnancy when your stomach takes longer to empty. Try to avoid spicy foods which can irritate your stomach and digestive system. Stick to good old bland foods.
It’s best to avoid fluids at meal time. Drink small amounts of fluids primarily in between meals instead. Don’t drink so much at once that your stomach feels full, as that will make you less hungry for food, although make sure you get plenty of water throughout the day to keep yourself well-hydrated, especially if you are vomiting. Sometimes drinks at cold temperatures help curb nausea better than hot drinks. Fruit juices, Gatorade and popsicles are helpful, as well as sucking on ice chips (an ice pack on your forehead might even help!) Keep caffeine intake to a minimum as it can make you feel worse, contribute to dehydration and further irritate nausea.
Many pregnant women crave sour or bitter tastes like lemon, which may have a therapeutic effect and can calm your system. Drinking lemonade or lemon water, smelling lemons, or just a small taste of lemon will normally calm an upset stomach. You can put slices of lemon in your iced tea, sparkling water or even simply suck on a lemon wedge.
Drinking decaffeinated herbal teas (be careful, some herbal teas may be harmful during pregnancy) may help relieve morning sickness. Teas like peppermint, mint, chamomile, red raspberry leaf and ginger can be calming in reasonable and small doses. Ginger is thought to settle the stomach and help relieve queasiness. Ginger ale (made with real ginger), ginger tea (grated fresh into hot water), ginger candies, dried ginger and ginger cookies may all help relieve nausea. Powdered ginger root capsules are another option. It is always advisable to speak to your doctor or midwife first before taking any herbs.
Sometimes, iron can be hard on your digestive system and become bothersome during pregnancy. Avoid extra iron supplements, especially in your first trimester, unless you are anemic. If you think your morning sickness may be related to your prenatal vitamins, talk to your doctor or midwife. They may switch you to a prenatal vitamin with a lower dose of iron for the first trimester. You might find that taking your prenatal vitamins later in the day, rather than in the morning may help. Also, taking them with food, possibly with dinner may be best, if they cause your stomach to be upset. Never stop taking your prenatal vitamin supplement, unless you’re advised by your doctor to do so.
Vitamin B6 eases nausea in some women and can be helpful in low doses. Increase vitamin B6 in your diet by eating whole grains, nuts, seeds, and legumes. Talk to your doctor or midwife about possibly taking a vitamin B6 supplement, because he or she can tell you how much to take and whether or not the amount in your prenatal vitamin should count as one of the doses. (The amount of vitamin B6 in supplements varies by brand.) Sometimes a combination of Vitamin B6 and Unisom are even more helpful in easing morning sickness. Never take any extra vitamin supplement without your doctor’s approval.
More Articles on Morning Sickness
—Morning Sickness
—Morning Sickness Help
—Diet and Morning Sickness
—Morning Sickness Alternatives


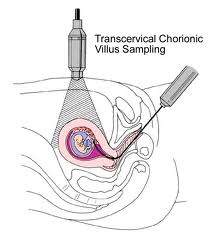 Chorionic villus sampling is usually done early in pregnancy between the 9th and 13th week. This is a procedure that involves removing a sample of chorionic villi cells from the placenta at the point where it attaches to the uterine wall.
Chorionic villus sampling is usually done early in pregnancy between the 9th and 13th week. This is a procedure that involves removing a sample of chorionic villi cells from the placenta at the point where it attaches to the uterine wall.
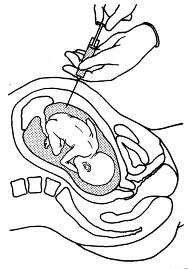 The amniocentesis test is a test in which a needle is used to remove a sample of fluid from the amniotic sac surrounding your baby. The amniotic fluid, which contains cell shed by your baby, is then studied in a lab for analysis. If done for chromosome analysis, amniocentesis is usually performed after the 16th week of pregnancy. If a woman needs to give birth early for some medical reason, amniocentesis might be done shortly before delivery to asses fetal lung maturity.
The amniocentesis test is a test in which a needle is used to remove a sample of fluid from the amniotic sac surrounding your baby. The amniotic fluid, which contains cell shed by your baby, is then studied in a lab for analysis. If done for chromosome analysis, amniocentesis is usually performed after the 16th week of pregnancy. If a woman needs to give birth early for some medical reason, amniocentesis might be done shortly before delivery to asses fetal lung maturity.




 Women with a higher intake of fat may be more likely to suffer morning sickness than those with less saturated fat. Limit or eliminate fatty, greasy and fried foods, which take longer to digest, particularly during pregnancy when your stomach takes longer to empty. Try to avoid spicy foods which can irritate your stomach and digestive system. Stick to good old bland foods.
Women with a higher intake of fat may be more likely to suffer morning sickness than those with less saturated fat. Limit or eliminate fatty, greasy and fried foods, which take longer to digest, particularly during pregnancy when your stomach takes longer to empty. Try to avoid spicy foods which can irritate your stomach and digestive system. Stick to good old bland foods.