In addition to cervical changes, temperature fluctuations, and changes in your cervical mucus during your monthly cycle, many women experience other fertility signals as well. Sometimes these additional symptoms are referred to as “secondary” fertility signs, because they don’t occur in all women, or even in every cycle in individual women. You can increase your chances of conceiving by familiarizing yourself with your emotional and other physical changes that occur each month and recording them on your chart in addition to your BBT, mucus and cervix signals. By doing this, you will get a more accurate picture of when you are most fertile.
Tag: tests
-
Fertility Charting
Fertility charting is basically a pregnancy achievement technique. It requires recording all of your fertility signs on a chart; allowing you to track ovulation, predict the most fertile time in your cycle, understand your own personal fertility patterns and increase your chances of becoming pregnant.
Besides rapid pregnancy achievement, charting can also be helpful in diagnosing and resolving many fertility issues, such as hormonal imbalance or ovulation problems. Potential complications that charting may be able to alert you on include anovulation (when no egg is released), low estrogen, low progesterone, thyroid conditions and even possible miscarriage.
For couples having difficulty in conceiving, fertility charting can be a very valuable tool. Charting can help you identify your most fertile days, so you can make love on those days to increase your chances of conception. A woman is only fertile for a few short days (the egg lives and can be fertilized for 12-24 brief hours after ovulation) during each menstrual cycle, so timing when you make love is critical part of conception.
In addition, many doctors and naturopaths strongly encourage fertility charting because it’s completely safe, natural and does not rely on drugs or medical procedures and there are no health risks or side effects. Plus, by charting your fertility, you will also become more aware of the patterns unique to your body, along with gaining a better understanding of how pregnancy is achieved. Once you understand these patterns and changes (and with a little patience), you can begin to anticipate ovulation through a combination of methods:
–Tracking your basal body temperature (or BBT)
–Observing changes in your cervical mucus
–Monitoring your physical and emotional symptoms
–Checking the position and shape of your cervixRead more on Fertility
-
More on Episiotomies (continued)
Many recent studies have shown that routine episiotomies shouldn’t be performed, because they are not helpful to the majority of women, although there are certain circumstances when they are needed. Having an episiotomy can increase pain during the postpartum period, leading to a longer recovery time. In addition, women who have episiotomies may have weaker pelvic floor muscles as well as more pain when resuming intercourse postpartum.
Episiotomy rates have declined over the years, but the number still remains high. Despite all the evidence against routine episiotomy use, close to 50- 80% of first time moms end up with an episiotomy in the U.S. The majority of women having them done are young white women, who have private insurance, according to a recent study.
There are a few situations when an episiotomy may be medically necessary. If there is a sign that your baby is in distress while in the birth canal, such as slowing of your baby’s heart rate, an episiotomy may be unavoidable for the sake of your baby’s well-being. If your baby’s shoulders get stuck, if your baby has a very large head that cannot fit through the vaginal opening or if delivery happens too quickly for the skin of your perineum to stretch naturally, you may need an episiotomy.
Perineal message helps reduce the chance of tearing during birth and the need for an episiotomy. It can make the perineum more flexible and increase elasticity, in preparation for birth. It’s a good idea to start doing perineal massage around the 34th week of pregnancy or before. To perform perineal massage, wash your hands thoroughly (or your partner). Place K-Y jelly, vitamin E oil or another mild lubricant on one or two fingers and gently stretch the lower part of the vagina until you feel a slight burning sensation. Hold the pressure steady for about 2 minutes or so. Repeat this daily for about 8-10 minutes.
Warm compresses during labor (especially during the pushing stage) encourage the stretching and relaxing of the perineum. Make sure they are only warm, but not hot, which can cause some swelling. Positioning during labor and birth may contribute to whether you need an episiotomy or not. Squatting can help reduce tearing. Avoid laying directly on your back, if possible and keep changing positions if you can. Talk to your doctor or midwife early about your feelings regarding episiotomies, especially if you wish to avoid one.
-
Emotional Fertility Signs
For fertility, charting your mood swings, thoughts, emotions and energy level along with your cervical mucus and changes, your other physical changes and your BBT, you may discover that they are closely linked to possible conception. On the other hand, some women don’t notice cyclic mood and energy variations whatsoever.
Estrogen rises and peaks as ovulation approaches, therefore many women experience increased sexual feelings, heightened desire, and more feelings of affection. This may be due in part to the increased slippery-feeling cervical mucus (which is similar to arousal fluid, but more watery) that is produced as ovulation draws near, causing increased libido on your most fertile days. It’s no coincidence that the word “estrogen”, the fertility hormone, stems from Latin roots which mean “creating mad desire.”
Other secondary signs you may notice as ovulation approaches may include: increased energy level, heightened sense of vision, smell or taste, easier concentration and mood swings. After ovulation, as your fertile phase ends, you may suddenly feel depressed or let down. Many times you may experience a drop in your libido as well. These feelings are important signals and are good to note on your chart.
-
Episiotomy
A small incision during delivery is an episiotomy. Right before your baby’s head emerges during delivery, in the pushing stage of labor, you may be given an injection of local anesthetic and your doctor or midwife may make a small incision in the skin between your vagina and anus (your perineum). This is called an episiotomy. An episiotomy is usually a second degree cut in both the skin and muscle of your perineum made for the purpose of enlarging your vaginal opening to assist in delivering your baby. The incision is closed with stitches after your baby and the placenta have been delivered. It is one of the most common medical procedures performed on women and also one of the most controversial.
There are two main types of cuts: a midline (the most common), which is a cut directly towards the anus and a mediolateral, which is a diagonal cut toward the side. The most common are second degree and the least common are fourth degree cuts.
Many doctors believe that an incision heals more easily than a tear. Other claimed benefits of episiotomy include prevention of possible third or fourth degree lacerations, lacerations that reach the anus, incontinence later on, damage to the pelvic floor and injury to the baby, as well as shortening the pushing stage; leading to a quicker delivery. Some doctors say that episiotomies are preferred, because they are simply easier to repair.
<<click here for the rest of the article on episiotomies.>> -

Maternal Serum Alpha-Fetoprotein (MSAFP) Test
This is a blood test which measures the level of alpha-fetoprotein (AFP) in your blood. It’s designed to indicate an increased risk for fetal open neural tube defects, such as spina bifida and may also indicate an increased risk for Down syndrome.
With the MSAFP Test there is a possibility of a “false negative” as well as a “false positive”, since no screening test is perfect.
This test is usually done between the 16th and 18th week of pregnancy.
More Tests
—Amniocentesis
—Chorionic Villus Sampling (CVS)
—Contraction Stress test (CST)
—Glucose Tolerance Testing
—Hemoglobin Test
—Non-Stress (NST) Test
—Rh Factor
—Triple Screen Test
—Ultrasound -

Hemoglobin Test
A protein found in red blood cells is called hemoglobin. By measuring your hemoglobin level during pregnancy, your doctor can determine whether you have anemia.
If you do become anemic, your doctor will advise you about changes in your diet and may recommend an iron supplement.
This test is normally done during your first prenatal visit, along with other lab work, but it may be done more often if you are found to be anemic.
More Tests
—Amniocentesis
—Chorionic Villus Sampling (CVS)
—Contraction Stress test (CST)
—Glucose Tolerance Testing
—MSAFPT Test
—Non-Stress (NST) Test
—Rh Factor
—Triple Screen Test
—Ultrasound -

Glucose Tolerance Test
This “Glucose Tolerance Test” is performed routinely to determine whether you have gestational diabetes.
Gestational diabetes is a form of diabetes that can develop in a pregnant woman who didn’t have diabetes before pregnancy. It is caused by changes in a pregnant woman’s metabolism and hormone production.
The risk of gestational diabetes is higher in women over 30, who have a family history of diabetes, or who are obese.
A glucose tolerance test is usually done between the 24th and 28th weeks of pregnancy. You will be asked to drink a glucose solution and after an hour, blood is drawn and the glucose level is checked. About 15 percent of pregnant women who are given a glucose tolerance test will have abnormal levels and a second test is done.
More Prenatal Tests
—Amniocentesis
—Chorionic Villus Sampling (CVS)
—Contraction Stress test (CST)
—Hemoglobin Test
—MSAFPT Test
—Non-Stress (NST) Test
—Rh Factor
—Triple Screen Test
—Ultrasound -
Contraction Stress Test
The “Contraction Stress Test” is another prenatal test used to help evaluate the condition of your baby and is often done when a non-stress test is non-reactive, or in some high-risk pregnancies to check whether the blood flow to the baby is adequate.
Just like the non-stress test, the contraction stress test is done during the third trimester.
The CST measures your baby’s heart rate in response to contractions of your uterus. The difference is that your doctor will be looking at the heart rate during uterine contractions, rather than in response to movements.
More Tests
—Amniocentesis
—Chorionic Villus Sampling (CVS)
—Glucose Tolerance Testing
—Hemoglobin Test
—MSAFPT Test
—Non-Stress (NST) Test
—Rh Factor
—Triple Screen Test
—Ultrasound -
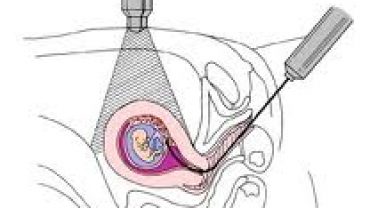
Chorionic Villus Sampling (CVS)
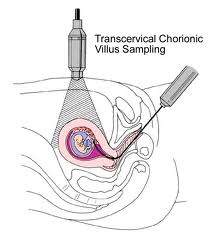 Chorionic villus sampling is usually done early in pregnancy between the 9th and 13th week. This is a procedure that involves removing a sample of chorionic villi cells from the placenta at the point where it attaches to the uterine wall.
Chorionic villus sampling is usually done early in pregnancy between the 9th and 13th week. This is a procedure that involves removing a sample of chorionic villi cells from the placenta at the point where it attaches to the uterine wall.In the more common trans-cervical method, ultrasound is used to guide a thin catheter through your cervix to the placenta. A small amount of chorionic villi cells are gently suctioned into the catheter. The trans-abdominal method is similar to amniocentesis and depends on ultrasound guidance. A long, thin needle is inserted through your abdomen into the placenta, where a small sample is withdrawn.
CVS is done for many reasons, but the main reason is for early detection of chromosome abnormalities, such as Down syndrome and other genetic disorders. CVS cannot diagnose neural tube defects because it doesn’t sample any amniotic fluid for testing levels of AFP.
The risk of a pregnancy ending in miscarriage are higher with CVS (one in 100) than with amniocentesis. Recent studies suggesting an association between CVS and limb malformation have made some doctors hesitant to offer this procedure.
Since CVS provides a larger sample of cells than amniocentesis, results take a little less time to obtain. Some results may be possible within a day or two.
More Prenatal Tests
—Amniocentesis
—Contraction Stress test (CST)
—Glucose Tolerance Testing
—Hemoglobin Test
—MSAFPT Test
—Non-Stress (NST) Test
—Rh Factor
—Triple Screen Test
—Ultrasound -

Amniocentesis
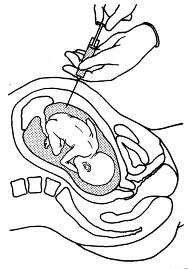 The amniocentesis test is a test in which a needle is used to remove a sample of fluid from the amniotic sac surrounding your baby. The amniotic fluid, which contains cell shed by your baby, is then studied in a lab for analysis. If done for chromosome analysis, amniocentesis is usually performed after the 16th week of pregnancy. If a woman needs to give birth early for some medical reason, amniocentesis might be done shortly before delivery to asses fetal lung maturity.
The amniocentesis test is a test in which a needle is used to remove a sample of fluid from the amniotic sac surrounding your baby. The amniotic fluid, which contains cell shed by your baby, is then studied in a lab for analysis. If done for chromosome analysis, amniocentesis is usually performed after the 16th week of pregnancy. If a woman needs to give birth early for some medical reason, amniocentesis might be done shortly before delivery to asses fetal lung maturity.In the first half of your pregnancy, your doctor may offer amniocentesis if your baby is suspected to be at increased risk for chromosome abnormalities, inherited disorders or neural tube defects. A chromosome analysis will also establish the gender of your baby (but amniocentesis is not offered for gender determination along.)
Amniocentesis is considered to be a relatively safe procedure. The risk of miscarriage caused by amniocentesis ranges from one in 200 to one in 400. In the rare instances tat amniocentesis causes a miscarriage, it is usually because an infection develops in your uterus, the water breaks or labor is induced prematurely. It is not uncommon for women to experience mild complications such as cramping or water leakage or discomfort around the needle site.
The procedure takes about 45 minutes. Your abdomen is cleansed with antiseptic. Some doctors offer a local anesthetic, which can be injected near the site to numb your abdomen. A long, hollow needle is placed through your abdominal wall and into your uterus. A small sample of fluid is withdrawn. Usually the results are back within a few days, although some require up to a week to obtain.
More Prenatal Tests
—Chorionic Villus Sampling (CVS)
—Contraction Stress test (CST)
—Glucose Tolerance Testing
—Hemoglobin Test
—MSAFPT Test
—Non-Stress (NST) Test
—Rh Factor
—Triple Screen Test
—Ultrasound -

Prenatal Tests
 The use of prenatal tests has become available since the 1980s and it can provide valuable information about the health of your baby.
The use of prenatal tests has become available since the 1980s and it can provide valuable information about the health of your baby.Prenatal testing can be helpful in determining any special care your baby may require during pregnancy and after he or she is born.
Knowing about birth defects before your baby is born can also help you and your partner prepare for any challenges ahead.
As you consider which prenatal tests are appropriate for you, think about the risks and benefits of each.
Types of Prenatal Tests
—Amniocentesis
—Chorionic Villus Sampling (CVS)
—Contraction Stress test (CST)
—Glucose Tolerance Testing
—Hemoglobin Test
—MSAFPT Test
—Non-Stress (NST) Test
—Rh Factor
—Triple Screen Test
—Ultrasound